Abstract
Introduction Sexual dysfunction and infertility have been described in patients with sickle cell disease (SCD) and may be related to sequelae of the disease itself or treatment. Hematopoietic cell transplantation (HCT) for SCD may prove to be curative, but has been associated with gonadal late effects including infertility. Data on long-term reproductive health outcomes after HCT for patients with SCD are limited.
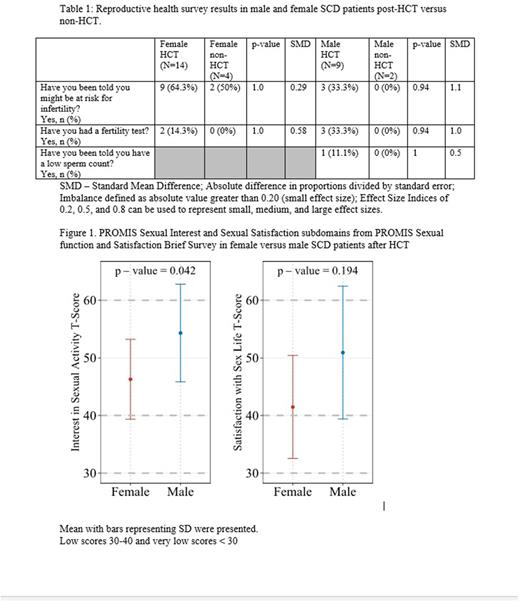
Methods We enrolled children and adults with SCD ³1-year post-HCT in the Sickle Cell Transplant Evaluation of Long-term and Late Effects Registry (STELLAR). Surveys were completed annually on a web-based platform. Patients who were ³18 years or proxy for patients <18 years completed surveys on risk for infertility. These questions were also completed by a comparison group of patients with SCD who had not had HCT. Individuals >18 years also completed the PROMIS Sexual Function and Satisfaction v2.0 Brief Profile (PSxFBP). Responses to the PSxFBP were in regard to the last 30 days and were reported on a 5-point Likert scale from 1 (none/never) to 5 (very/always). Descriptive statistics were reported as mean (min, max), median (Interquartile range: 3rd quartile - 1st quartile) or mean (standard deviation), and count (percentage). Statistical procedures involved chi-squared test, and effect size was calculated using standard mean difference (SMD). All PSxFBP subdomains were transformed on a T-score metric against the U.S. average population (0-100 scale with mean of 50 and SD of 10). T-scores 40-60 were normal, 30-40 low, and <30 very low.
Results Reproductive health surveys were completed by 23 patients with SCD who had HCT (14 F and 9 M) and 6 control patients with SCD (4 F and 2 M). Median (IQR) age at and time since HCT was 11.3 (6.5) and 5.9 (9.5) years in females and 12.8 (7.6) and 7.0 (11.5) years in males. Year of HCT from 2010-2020 (F: 71.4%, M: 55.6%), with matched related (F:78.6%, M: 88.9%) bone marrow (F: 85.7%, M: 88.9%) following myeloablative conditioning (F: 78.6%, M: 100%). One patient in each group underwent autologous gene therapy. Patients reported having been told they might have infertility in 9 (64.3%) females and 3 (33.3%) males post-HCT, compared to 2 (50%) female and no male non-HCT controls. Medical tests to inform fertility status had been completed in 2 (14.3%) females and 3 (33%) males post-HCT, with no tests reported in non-HCT controls. Only 1 (11.1%) male SCD HCT reported being told he had a low sperm count. SMD and p-values can be found in Table 1. The PSxFBP was completed by 10 females (mean age 23.7 years, range 21.0-27.9) and 8 males (mean age 25.3 years, range 19.1-38.3) post-HCT. In females and males, survey respondents were a median (IQR) of 11.6 years (8.7) and 8.9 years (14.0) years post-HCT, respectively. Most patients underwent matched related (F: 70.0%, M: 87.5%) bone marrow (F: 90.0%, M: 87.5%) HCT following myeloablative conditioning (F: 70.0%, M: 100%), with year of HCT 2010-2020 (F: 50.0%, M: 50.0%) and before 2010 (F: 40%, M: 25%). One patient in each group underwent autologous gene therapy. When asked about interest in sexual activity (Figure 1), mean (SD) T-scores were significantly lower in females than males at 46.3 (6.9) and 54.3 (8.5), respectively (p=0.042). A low T-score (30-40) was found in 3 (30%) of females and in 1 (12.5%) of male. There were no very low T-scores (<30). Sexual activity was reported in 40% of females and 100% of males. When asked about satisfaction with their sex life, there was no difference in mean (SD) T-score between females (41.5 [8.9]) and males (50.9 [11.5]; p=0.194). Low satisfaction T-scores were reported in 2 (50%) of females and 2 (28.6%) of males, and there were no very low T-scores (<30). Over half of the post-HCT males reported not attempting sexual intercourse, although 87.5% reported always being able to achieve an erection.
Conclusions After HCT, one-third of females and two-thirds of males reported a lack of awareness of their risk for infertility. In the transplanted cohort, the mean T score for the sexual interest subdomain was significantly lower in females than males but both were in the normal range. Sexual activity was reported in less than half of females but all males. The mean T scores for the sexual satisfaction subdomain were normal for females and males, but half of individual females and one quarter of the males had low T scores. Continued data collection will allow better characterization of the reproductive health in this population.
Disclosures
Pecker:GBT: Research Funding; Novo Nordisk: Consultancy; Global Blood Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal